As Medicare and Medicaid enrollment continues to expand and regulatory requirements grow more complex, payors are facing increasing operational challenges in identifying, enrolling, and retaining dual-eligible members. Manual processes, fragmented eligibility data, rising acquisition costs, and compliance obligations have made it difficult for organizations to scale Dual Eligible Special Needs Plan (D-SNP) programs efficiently.
Right Skale Inc. today announced the availability of DualEnroll AI, an artificial intelligence–enabled platform designed to help payors modernize and operationalize the dual enrollment lifecycle. The platform is intended to support eligibility identification, enrollment workflows, and ongoing recertification while aligning with applicable regulatory and compliance requirements.
Addressing Operational Complexity in Dual Enrollment
- Payors managing dual enrollment programs often contend with:
- Disparate eligibility data across federal, state, and internal systems
- Manual, time-intensive enrollment workflows
- Increasing customer acquisition costs
- Evolving CMS and state-level compliance requirements
- Inconsistent member experiences that can affect enrollment and retention
As competition for eligible members increases, many organizations are evaluating technology-driven approaches to improve efficiency and reduce administrative burden.
DualEnroll AI Platform Overview:
DualEnroll AI applies automation and data intelligence across key stages of the dual enrollment process. According to Right Skale, the platform is designed to integrate with existing payor systems and support enrollment operations without requiring major changes to current infrastructure.
Key platform features include:
- AI-assisted identification and prioritization of eligible members
- Automated enrollment and recertification workflows
- White-label deployment options
- API-based integration with core payor systems
- Security and compliance controls aligned with HIPAA, SOC 2, and CMS requirements
- Observed Outcomes from Early Deployments
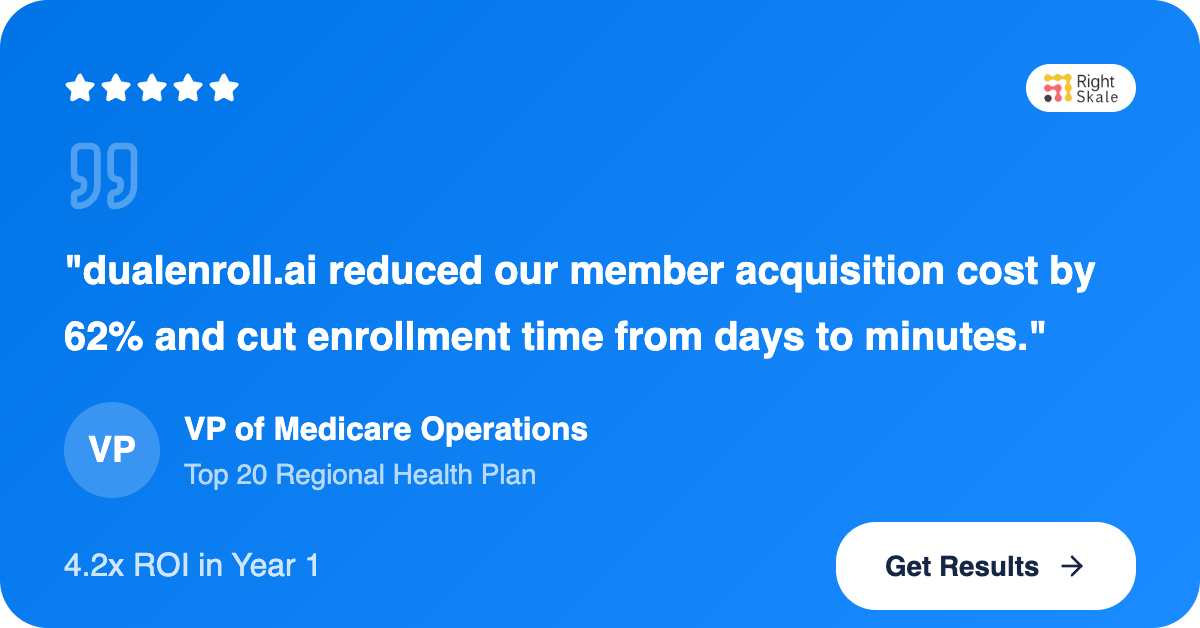
Right Skale reports that payors using DualEnroll AI have observed:
- Shorter enrollment cycle times
- Reduced administrative and acquisition costs
- Improved operational consistency
- Increased audit readiness across enrollment processes
Actual results may vary based on deployment scope, member population, and operational environment.
“Dual enrollment programs require both operational precision and regulatory discipline,” said a spokesperson for Right Skale. “DualEnroll AI was developed to help payors manage complexity more effectively while supporting scalable growth initiatives.”
Looking Ahead -
As CMS guidelines and state policies continue to evolve, payors are increasingly seeking platforms that can adapt to regulatory change while supporting operational scale. DualEnroll AI is designed to support current enrollment requirements while providing flexibility for future program expansion.
Learn More
Payors interested in learning more about DualEnroll AI or requesting a demonstration can visit:
https://rightskale.ai/dual-enrollment
Media Contact:
[email protected]
#Medicare #Medicaid #DualEligible #HealthcareEquity #SeniorCare #Veterans #HealthcareAI #EnrollmentAutomation #HealthcareInnovation #ValueBasedCare #PayerLeadership #RightSkale
DualEnroll.ai, powered by Right Skale, is designed to help Medicare and Medicaid payors modernize enrollment. Because access delayed is care denied — and every American deserves healthcare without worry.
? Learn more about how we can make coverage easier for our elders:
www.rightskale.ai/dual-enrollment